What Physical Conditions Encourage Skin Breakdown In A Patient Who Is Confined To Bed
Skin Health: Prevention and Handling of Pare Breakdown
Originally Published in The Siegel Rare Neuroimmune Association Journal
Book V
January 2011
Janet Dean, MS, RN, CRRN, CRNP
The International Center for Spinal Cord Injury
Kennedy Krieger Institute, Baltimore Maryland
Pare is the largest organ covering the entire outside of the torso. Information technology receives i tertiary of the trunk's blood circulation. Your skin is tough and pliable, forming the body's protective shield against oestrus, lite, chemic and physical activeness. It plays an agile role with the immune system, protecting us from infection. Your peel maintains a stable internal environment and is of import in maintaining a proper temperature for the body to office well. In improver to providing protection and internal regulation, your skin gathers sensory information from the environment, allowing you to feel painful and pleasant stimulation. Your peel also stores water, fat, and vitamin D.
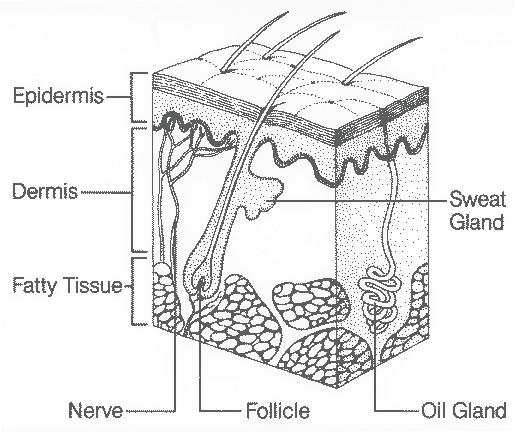
The pare consists of 3 layers: Epidermis, dermis, and subcutaneous tissue. The outermost layer, the epidermis, is equanimous mostly of expressionless skin cells that are constantly being shed and replaced. The dermis or second layer has sweat glands, oil glands, nervus endings, and small claret vessels called capillaries, which are all woven together by a protein called collagen. Collagen provides nourishment and back up for skin cells. The nerves ending in this layer transmit sensations of pain, itch, touch and pleasance. The hair follicles too originate in this layer. Destruction of either the epidermis or dermis tin can leave the torso open up and susceptible to infection. The subcutaneous adipose tissue is the deepest layer of skin and is a layer of fat and collagen that houses larger blood vessels and nerves. This layer is of import in decision-making the temperature of the skin itself and the torso and protects the body from injury by acting as a shock absorber. The thickness of this layer varies throughout the body and from person to person. Underneath the subcutaneous tissue lays muscle and bone.
For the nigh role, the skin is tough, pliable and resistant to injury. If the skin becomes injured or broken, it is generally very resilient and has an amazing power to self-repair and heal. Despite this resiliency, the skin is susceptible to breakdown, if subjected to prolonged abuses, such as excessive pressure level, shear force, friction or moisture. This is a major business for persons with transverse myelitis or other neuroimmunologic conditions that cause paralysis and/or decreased awareness.
For people with paralysis, the skin is at increased risk for breakdown for several reasons. Paralysis itself affects the skin and underlying tissue. At that place is loss of collagen which weakens the skin and makes it less rubberband. The lack of musculus function around boney areas of the torso leads to muscle cloudburst, resulting in less padding, which in turn, adds to the risk of skin breakdown. People with paralysis frequently have difficulty shifting their weight, repositioning themselves, or transferring without assistance.
Impaired sensation is frequently present, limiting the ability to sense when to make a weight shift or position adjustment. People with impaired sensation are also vulnerable to injury from many other hazards, such equally, heat, cold, sun and trauma. Loss of sensation put an individual at take chances for burns from very ordinary activities, such as using a lap superlative computer sitting straight on your lap or sitting too shut to a fireplace. Injury can exist acquired from things that are too common cold such as, water ice packs or cold exposure causing frostbite. Ingrown toenails tin can get infected and sunburn can become severe without feeling it.
When limited mobility is coupled with decreased sensation, a person is more than likely to develop a specific blazon of pare breakdown called a force per unit area ulcer. According to the National Force per unit area Ulcer Advisory Panel, a pressure level ulcer is defined as a localized injury to the peel and/or underlying tissue usually over a bony prominence, every bit a outcome of pressure level, or pressure level in combination with shear and/or friction (1). Pressure ulcers are one of the leading causes of complication across the life span of persons with paralysis (2). Up to 95 % of adults with spinal cord injury will develop at least one serious pressure level ulcer at some fourth dimension during their life (three).
Peel breakdown can range from minor scrapes, cuts, tears, blisters or burns to the most serious force per unit area ulcers with the destruction of tissue down to and even including the os. A force per unit area ulcer, specially ane that requires surgery, such as a musculus flap or peel graft, tin can cost thousands of dollars to treat, crave lengthy hospitalization, and weeks to months away from family, work, schoolhouse or community activities. It has been estimated that for persons with spinal cord injury the cost of intendance for pressure ulcers is nearly $1.two to i.3 billion dollars annually (4).
With a concerted effort, skin breakdown is, for the most part, preventable. It can occur, however, even in people who maintain the most diligent care and use the proper equipment. If skin breakdown is identified early, when still in the minor stages, and if the cause of the breakdown can exist identified and eliminated, healing should occur fairly speedily. If it is not identified in its early on stages, pare breakdown tin speedily progress from modest to serious.
Pare breakdown is caused in several different means, including friction, shear, wet and pressure. These causes can occur individually or in combination. Friction, moisture and sheer are identified equally contributing factors to pressure ulcers (v). A friction injury occurs when the skin rubs on surfaces, such every bit a bed canvass, arm residuum or brace and has the appearance of a scrape, chafe or blister. This type of injury is typically seen on the heels and elbows and may event from repositioning, propping or rubbing due to increased spasticity.
A shearing injury occurs with dragging or sliding of a body part beyond a surface and has the appearance of a cut or tear. This type of injury can occur from dragging your lesser during a transfer or sliding downwards in bed when the head of the bed is elevated. With the sliding force, bone is moved against the subcutaneous tissue while the epidermis and dermis remains essentially in the same position; against the supporting surface such as a wheelchair or bed. This activeness causes occlusion of the blood vessels, decreasing blood flow, oxygen and nourishment to the skin, which eventually leads to breakup. Sometimes a shear injury will actually tear the tissue over the tailbone and with unrelieved pressure volition go a pressure ulcer.
Besides much moisture over-hydrates the skin, making it weak and more sensitive to friction, shear and breakdown (remember about being in the tub or puddle for a long time). Primary sources of excess skin moisture include sweating, bowel and bladder accidents, and drainage from wounds.
Force per unit area ulcers occur when skin, soft tissue and claret vessels are compressed or squeezed between a bony prominence (such as your tailbone) and an external surface (such every bit your wheelchair absorber). With compression of these vessels, the blood that nourishes the cells and takes away waste product is cut off, starving the tissue of oxygen and vital nutrients. Without food and oxygen, tissue dies and peel breakdown begins. The trunk tries to recoup by sending more blood to the area. This procedure results in redness and swelling, places even more pressure on the blood vessels, and further endangers the health of the skin and underlying tissue. Ultimately, a pressure ulcer forms. Increased pressure over short periods of fourth dimension and slight pressure over long periods of time have been shown to crusade equal amounts of impairment.
Many factors have been identified equally responsible for the evolution of pare breakdown and pressure ulcer germination. In addition to immobility, dumb sensation and the external factors described above, many internal contributing factors have been identified. These internal factors include poor nutrition and hydration, weight, impaired circulation and oxygenation, dumb cognition or thinking, substance abuse, low and historic period (6, 7). Nutritional factors important to prevent or heal wounds include a balanced diet with an adequate intake of protein, vitamin C, vitamin A, and zinc, besides as an adequate intake of fluids (eight). When a person is overweight, actress pounds identify extra pressure level on vulnerable pare areas increasing the gamble of compression of blood vessels. Individuals that are underweight ofttimes have decreased muscle mass with less fatty padding over boney areas leaving them vulnerable to peel breakdown. Smoking, diabetes, anemia and other vascular conditions all lead to decreased circulation, increasing risk for pare breakdown. Individuals who are depressed or take impaired thinking and judgment due to substance abuse are less likely to exist vigilant with regard to important self-care issues, such as skin health. Young children more often than not have more resilient and rubberband peel and more infant fat and padding so they oft have very little difficulty with skin interruption down. As children movement into adolescence, their skin loses some of its elasticity. They generally have more than body weight, putting more stress on pressure areas, such as the ischeal tuberosicties and tailbone with sitting. Teens often begin to accept more difficulty with skin breakdown. Equally nosotros continue to age, our skin becomes increasingly less pliable and resilient. Nosotros experience the loss of collagen and muscle mass, as well as decreased apportionment, making the skin more vulnerable. The elderly are well-nigh decumbent to skin tears and stripping due to delicate, thin, and vulnerable skin. In addition, incontinence may get a more than frequent issue for bedridden or ill persons, increasing issues with moisture as described to a higher place.
How can I keep my skin healthy?
Accept responsibleness for you ain peel intendance
The first line of defense force in keeping your skin healthy is to have responsibleness for your own skin care. If yous are at take a chance for skin breakdown, yous will demand to develop a daily routine for monitoring and caring for your peel. You lot should practice a consummate inspection of your pare every day. If you lot are unable to assess your ain peel, you should be knowledgeable about the areas of your body where you are most vulnerable to skin breakdown and be certain that your care givers are checking these areas for you and reporting the condition of your pare.
The most common areas for skin breakdown (pressure points) in adults are the sacrum/coccyx (tailbone), heels, elbows, lateral maleollus (exterior of the ankle), greater trocater (hip os) or the lesser of the femur (outside and inside of the knee) and the ischial tuberosities (the bones we sit down on). Force per unit area points for children are different and based on age and development (vii). For infants and children less than 3 years of historic period, the head makes up a greater portion of the total torso weight and surface areas. When they are placed on their backs, the occipital region (back of the head) becomes the primary pressure indicate. When placed on their side, the ears are also very susceptible. For older children, the sacrum (lower spine) and calcaneous (the heel of the human foot) are most at risk (9).
Teach children to take responsibility for their own skin intendance
Parents of children at chance for pare breakdown need to be sure to bank check their children's peel every mean solar day. This can get more than difficult as children enter their teen years, develop more than modesty and are interested (or insistent) on being more independent in their own care. This may be an area that parents need to insist on participation as skin breakup can progress from minor to serious literally overnight in a child (or in an developed for that matter). If y'all have made daily skin inspection a part of your child'south routine since the onset of paralysis, this should be less of an effect. Be sure that they have the equipment, such equally a mirror on a flexible wand, to inspect their ain skin with your oversight, if at all possible.
Forbid mechanical Injury
Prevent mechanical injury to the peel from friction and shearing forces during repositioning and transfers. Elevator, don't slide. Lowering the caput of the bed will help minimize sheer and friction from sliding down in bed. Raise the entire bed upward to the proper meridian to facilitate level surface transfers to and from a wheelchair. If necessary, utilise assistive devices, such every bit transfer boards or mechanical lifts to help with transfers. Your concrete or occupational therapist can assistance y'all with training and obtaining the correct equipment. Ensure that article of clothing fits comfortably and does non have force per unit area points, such as snaps, thick seams or pockets. Be sure that article of clothing is smoothed downward under the bottom and back then you don't get pressure level points from bunched fabric. Keep bed sheets every bit wrinkle costless as possible.
Keep skin clean and dry
Breast-stroke ofttimes using balmy soap. Avoid very hot water equally it dries skin. Dry out your skin past patting rather than rubbing. Alter undergarments or pads as soon every bit possible afterward a bowel or bladder accident.
Eat a good for you diet
Eat a healthy diet and potable lots of fluids, especially water. Keep your body weight in a healthy range. People that are overweight or underweight tend to have more issues with skin breakdown. Good nutrition volition help make your skin more than resistant to breakdown and you will be more than likely to heal and fight off infection should it occur. Eat the right kinds of foods. This means a balanced diet with servings from all nutrient groups. For healthy pare it is especially of import to go enough of the following nutrients in your diet:
- Omega 3 fatty acids (salmon, mackerel, flaxseed)
- Vitamin C (citrus fruits, strawberries, broccoli)
- Vitamin A (Vegetables that are night green or dark orange in color)
- Zinc (seafood, meat and eggs)
- Protein (meat, eggs, cheese, and soy products)
Extra calories, specially from protein, are important for repairing damaged tissues if you do take skin breakdown. If y'all are concerned that you do not go plenty of these foods in your diet, you can speak with a nutritionist or your health intendance provider virtually supplementation.
Develop a good domicile rehabilitation plan
A regular daily therapy program will contribute to your overall health and well being, as well every bit reduce the risk of skin breakdown. A good program should include therapy to increment muscle mass and strength, improve your flexibility, improve your cardiovascular endurance, and increment your circulation. An activity based program that includes components of weight bearing and/or gait training, functional electrical stimulation biking, as well as strengthening and stretching activities are benign to help prevent skin breakdown. Utilize of the Wii gaming system in artistic ways for "Wiihab" can help with improving strength, balance and endurance. Aquatic therapy and horseback riding therapy are besides beneficial, in add-on to being fun.
Avert prolonged pressure on any i spot
Reposition frequently. When seated in a wheelchair, do weight shifts every 15 minutes. When lying in bed, reposition every 2 – 4 hours. Utilize pillows or wedges backside your back and between bony areas, such every bit knees and ankles. "Bladder" your heels and ankles off of the bed by supporting your lower leg with a pillow. Go along the head of the bed up less than 30 degrees to prevent shearing of pare from sliding downwardly or the need to be pulled back up. If you use a wheelchair nigh of the day, avoid lying on your back at nighttime. Instead, turn side to side to give your backside a break. Better however, sleep on your stomach, if this position is comfy and y'all are able to breathe safely. When positioned on your tum, you have fewer pressure level points, and tin by and large turn less frequently. Beingness on your stomach gives your backside a break, and allows you to stretch your hip flexor muscles and hamstring muscles, all for the toll of one!
Utilize therapeutic surfaces
Therapeutic surfaces, such as a pressure relieving wheelchair absorber or a force per unit area relieving mattress will reduce or relieve pressure, promote blood flow to tissues and enable proper positioning. Make sure that you use equipment the way it is recommended and that it fits correctly. When seated in a wheelchair, make certain the cushion is properly positioned and inflated and that you lot are sitting all the way back in the wheelchair.
Keep muscle spasms under control
Some muscle spasms can exist beneficial as they help you change position, if you can't move yourself. Too much muscle spasticity tin can cause rubbing and friction, especially when you are in bed at nighttime. Talk with your care provider about how to all-time manage spasticity. Practice and range of motion are ii good ways to reduce spasticity. Brand certain orthotics (braces) are fitting properly, that they are worn correctly, and that the straps are fastened properly to prevent friction or pressure. Exist sure that your float and bowel programs are working well as increased spasticity can be caused by a urinary tract infection or constipation. Spasticity can besides increase when yous have a burn or peel breakup.
Identifying and treating minor pare breakdown
What does minor peel breakup look like?
Skin breakdown starts out equally a red or purple spot on fair skin or a shiny, purple, bluish or darker spot on nighttime skin, which does not fade or go away within 20 minutes. When y'all printing on the spot with your finger, it does not go lighter (blanch). Information technology may feel warmer or libation than the skin around it. The spot may feel hard or squishy under your fingers and may look swollen. If you take sensation, information technology may exist itchy or painful. At get-go, information technology may not look like much, peculiarly if the skin is non broken or open, but information technology can go a lot worse. If your skin becomes blistered, scabbed or has a small open area on the surface, this is more serious, as it indicates that the tissue underneath has begun to die. At this stage, the progression of skin break down is reversible: the skin volition render to normal every bit shortly equally the cause of the irritation is establish and eliminated and the peel is properly cared for. If these steps are not taken, the damage can rapidly progress to a unsafe level where infection can attack the underlying tissue and bone, posing a serious risk to your health.
Treating redness or minor peel breakdown
If the pare is open, contact your health care provider for wound care instructions. These instructions will generally include cleaning the area with soap and water or a saline solution, keeping the area dry, and eliminating the cause of the trouble. Do non utilise hydrogen peroxide or iodine as these products damage new pare cells in the wound. They may prescribe special dressing that will optimize healing. If not, encompass the surface area with a non-stick dressing, such as a Telfa pad to protect it from habiliment. Modify the dressing one to ii times per day or if it gets soiled. Bank check your peel oft to be certain the area is not getting worse. Small-scale burns can too crusade blistering and can exist treated in the same mode. If the fire covers a large surface area, you should seek care in the emergency room. Once a treatment plan has been established, you must identify and try to remove the source of the irritation to the afflicted area as much equally possible.
Is the damage being caused by force per unit area during sitting?
Pressure level areas caused by sitting ofttimes occur on your ischeal tuberocities (sitting basic), lower dorsum, shoulder blades or the back of the heels. If the skin sore is being caused past sitting, check your wheelchair cushion. Do you take a pressure relieving cushion prescribed past your wellness care provider? Is it inflated correctly? Some cushions require frequent monitoring of inflation and can leak. Could the cushion be placed backward in the chair? Is it in good repair? Some cushions have gel in them that tin can get hard or squished out of place. If you lot have a therapeutic cushion and are yet having difficulty with pressure on your sitting basic, meet if you tin can try dissimilar cushions with pressure mapping. Pressure mapping equipment allows clinicians to visually identify your specific pressure level areas when sitting on dissimilar cushions. Then the cushion that works best for you tin be ordered. Pressure mapping can too exist helpful, if you have a condition that can make seating hard. Weather, such as scoliosis or a dislocated hip can make the pressure level on you lot sitting basic unequal. Depending on how bad the skin breakdown is you may need to stay out of your wheelchair for a period of time to allow the area to heal.
Is the impairment being caused by pressure from lying on the area?
The areas about vulnerable when lying are the dorsum of the head (in young children), ankles, knees, hips or shoulder blades. If then, avoid positioning on the afflicted area. If yous take difficulty with reddish areas despite frequent turning, there are various pressure relieving mattresses that can be prescribed past your wellness intendance provider to distribute pressure better than a regular mattress. Unfortunately, if you lot take never had whatsoever skin breakdown, information technology is hard to get insurance coverage for this type of specialty mattress. If you take had peel breakdown, coverage is often bachelor.
Does the expanse of damage look more like a scrape or a tear?
If the area looks more similar a scrape or tear, it may be caused by friction or sheer from sliding downwardly in bed or wheelchair or from dragging your bottom with transfers. If you lot have had a change in your physical status, consider returning to physical therapy for a "tune up" focusing on increasing your strength, flexibility, and transfer technique. If you lot are dependent on others for part or all of your transfers, there is equipment that can be helpful to preclude sheer injury. This includes transfer boards, starting with simple slippery wood boards to a b-easy lath with a sliding deejay, a mechanical lifting device or overhead track elevator systems. Your physical therapist and occupational therapist can assist you lot place equipment that will be nearly helpful for yous and teach you lot and your care givers how to safely use this equipment. A hospital bed that raises and lowers and has an elevating head and foot remainder tin be helpful, specially if yous require help from others for bathing, positioning and transfers. The ability to enhance and lower the bed will protect your caregiver'south back and often allows for level or "downhill" transfers, avoiding sheer injuries. Transmission (hand crank) hospital beds or semi-electric hospital beds (hand creepo to raise and lower the bed and electric to elevate the caput and human foot) are oft covered by insurance with a skillful letter of medical necessity from your wellness care provider. Inquire your health intendance provider to social club a fully electric infirmary bed, if y'all are unable to operate a paw crank independently. Your health care provider should indicate that you lot require assistance with transfers and bed mobility and crave frequent repositioning to prevent costly skin breakdown. If y'all prefer not to accept a hospital bed, you tin can permanently raise the height of your entire bed then that it is even with your wheelchair using blocks of wood, bricks or bed leg adjusters that can exist purchased.
Is the surface area of damage under a brace?
If redness persists greater than twenty minutes after removing the brace, do not wear the brace. Have your therapist or orthotist evaluate the brace to see if it can be adjusted or whether it will need to exist remade. Children may need adjustments or replacement of braces as often every bit every four to half dozen months during growth spurts. Braces will oft crave aligning, if you have lost or gained weight, have increased spasticity, decreased range of motility or worsening scoliosis.
Is the redness or breakdown in the diaper (perineal) surface area?
Skin breakdown in the perineal area is generally caused by too much wet oftentimes from sweating or irritation from urine and stool. Peel problems in this surface area start out equally redness and swelling (rash) and can progress to vesicles or pimples with oozing, crusting or scaling. Once the skin is open, there is increased risk for infection. Perineal skin care should be done as presently as possible after a bowel and/or bladder accident. Gently wash the area with soap that is indicated for the perineal area. Regular bar soap or antibacterial soap used for routine peel intendance tin can dry this skin. The skin in this area will need moisturization with products such equally glycerin, lanolin or mineral oil to replace natural moisture that is lost with frequent cleaning. A pare bulwark ointment or creams should exist used to protect the skin from wet or irritation.
If the redness or rash last longer than three days, has areas of multiple red bumps or pimples, or if you have oozing pimples that develop into a dearest-colored crusted area, you should exist seen by a heath professional as you may demand handling for a yeast infection or an antibody. Under-pads or absorptive briefs can exist used as long as they wick moisture away, rather than trapping the moisture against the peel. Lastly, try to identify the crusade of the peel irritation, particularly if from frequent bowel or bladder accidents.
Identifying and treating serious peel breakdown
What does serious pare breakup look similar?
Serious peel breakdown occurs when the crusade of the problem is not eliminated and tissue has been deprived of oxygen and nutrients for so long that the tissue has died and there is now a big pigsty or crater. Harm extends at to the lowest degree into the subcutaneous tissue. In the nigh serious wounds, tissue death includes muscle and extends as deep equally the bone. Drainage is almost always present. If you have fever, see green or yellow drainage, and have a warm temperature around the wound, you may have adult an infection. Wounds such as this, with or without infection, must exist evaluated by a health care professional. This care may exist obtained through your spinal string injury provider or you may exist referred to a wound center to be evaluated and treated past a professional person that specializes in the treatment of serious wounds. When an infection forms in a wound, the surrounding tissue and os can become infected. If this continues, infection can enter the blood stream causing sepsis; and if untreated, can be fatal.
How is serious skin breakdown treated?
If the wound is not infected, you may be able to be treated at domicile with bed residual and frequent dressing changes. You should be evaluated past a wound care professional to identify the appropriate handling plan and dressings. Specialized dressings are of import to provide a moist environment for healing. Moist wounds heal faster than dry wounds. It is easier for a wound in a moist environs to comminute or grow new cells and for the cells to motility across the wound bed. A moist surround increases the effectiveness of white blood cells in fighting infection, removing waste and expressionless tissue. Specialized dressings are also of import to be sure that the wound heals from the inside out. If the wound heals from the exterior first, it can trap infection inside that will later flare up and cause the wound to reopen. Deeper wounds need specialized wound care, including the removal of dead tissue either by special wound dressing or ointments (chemical debridement) or surgical removal of this tissue. This volition then exist followed past special dressings and packing material that can absorb drainage, remove dead tissue and so assist the body heal itself. If a wound is draining heavily, a special dressing should be used to comprise the drainage.
The most serious wounds, those that extend to the os or take signs of infection, will require hospitalization for treatment. This will mean several weeks of bed residual with ambitious wound management and 4 antibiotics. Aggressive handling in a hospital that has a specialized wound care squad can help yous avoid surgery. Newer wound treatment and dressings can speed healing. Many hospital and wound centers use vacuum assisted closure therapy, hyperbaric oxygen therapy and electric stimulation either directly in the wound or in the tissue surrounding the wound. Electric stimulation should non be used if in that location is whatever run a risk that the underlying bone may be infected (osteomyelitis). If non-surgical treatment fails, or the wound is very severe, surgery volition be required. Nearly often this volition involve a muscle flap and skin grafting to shut the wound and forestall reoccurrence of skin breakup. This type of surgery generally costs thousands of dollars and requires a period of weeks in the infirmary followed by several more than weeks at domicile or in the hospital on a specialized bed. The total process is oftentimes half-dozen – 8 or 10 weeks before you can begin a gradual reseating program.
Conclusion
While it is well know that preventing skin breakdown is much easier than treatment and that at that place are many identified risk factors that tin can be modified to prevent skin breakdown, we know this is only part of the upshot. In the real globe, even with the best self-care or the best caregivers, y'all tin develop skin breakdown if unexpected events or changes in your life occur. Call up, the threat of pare breakdown never subsides and, in fact, increases with aging and with the length of time from your diagnosis or injury. Information technology is easy to go over confident or even lax in maintaining prevention habits the longer y'all take gone without having skin breakdown. Exist increasingly vigilant with unexpected changes in your circumstance. Changes, such the loss of a trusted intendance giver or increasing responsibilities at home, piece of work or school, tin can increment the risk to your skin. Sudden breakage of equipment as well places you at increased risk. Being proactive and assertive in monitoring, maintaining and replacing broken or worn out equipment, such as wheelchair cushions is very important. Lastly, if you accept a problem with skin breakdown, take accuse immediately. Seek out professional person help before it becomes serious.
Reference listing
- National Pressure Ulcer Advisory Panel. Updated staging system of the national pressure ulcer advisory panel. Feb, 2007. https://world wide web.npuap.org/pr2.htm. Last accessed December 3, 2010.
- Krause JS, Carter RE, Pickelsimer EE, Wilson D. A prospective study of wellness and risk of mortality later on spinal cord injury. Arch Phys Med Rehabil. 2008;89:1482-91.
- Jackson J, Carlson M, Rubayi S, Scott Md, Atkins MS, Blanche EI, Saunders-Newton C, Mielke South, Wolfe MK, Clark FA. Qualitative study of principles pertaining to lifestyle and pressure level ulcer gamble in adults with spinal cord injury. Disabil Rehabil. 2010;32(7):567-78.
- Regan MA, Teasell RW, Wolfe DL, Keast D, Mortenson WB, Aubut JA, Spinal Cord Injury Rehabilitation Evidence Inquiry Team. A systematic review of therapeutic interventions for pressure ulcers after spinal string injury. Arch Phys Med Rehabil. 2009;90(2):213-31.
- Garber SL, Rintala DH. Pressure ulcers in veterans with spinal string injury: a retrospective study. J Rehabil Res Dev. 2003;twoscore(5):433-41.
- Jackson J, Carlson M, Rubayi S, Scott Medico, Atkins MS, Blanche EI, Saunders-Newton C, Mielke Due south, Wolfe MK, Clark FA. Qualitative study of principles pertaining to lifestyle and force per unit area ulcer adventure in adults with spinal cord injury. Disabil Rehabil. 2010;32(7):567-78.
- Butler CT. Pediatric skin care: Guidelines for cess, prevention, and treatment. Ped Nurs. 2006;32(five):443-450.
- National Force per unit area Ulcer Advisory Panel. The function of diet in pressure ulcer prevention and treatment: National pressure ulcer informational console white paper. 2009. https://www.npuap.org/
- Baharestani MM, Ratliff CR. Pressure ulcers in neonates and children: An NPUAP white paper. Advan Skin & Wound Care. 2007;20(4):208-220.
Source: https://wearesrna.org/resources/skin-health-prevention-and-treatment-of-skin-breakdown/
Posted by: albertwomilorge.blogspot.com

0 Response to "What Physical Conditions Encourage Skin Breakdown In A Patient Who Is Confined To Bed"
Post a Comment